Conditions
Cardiology
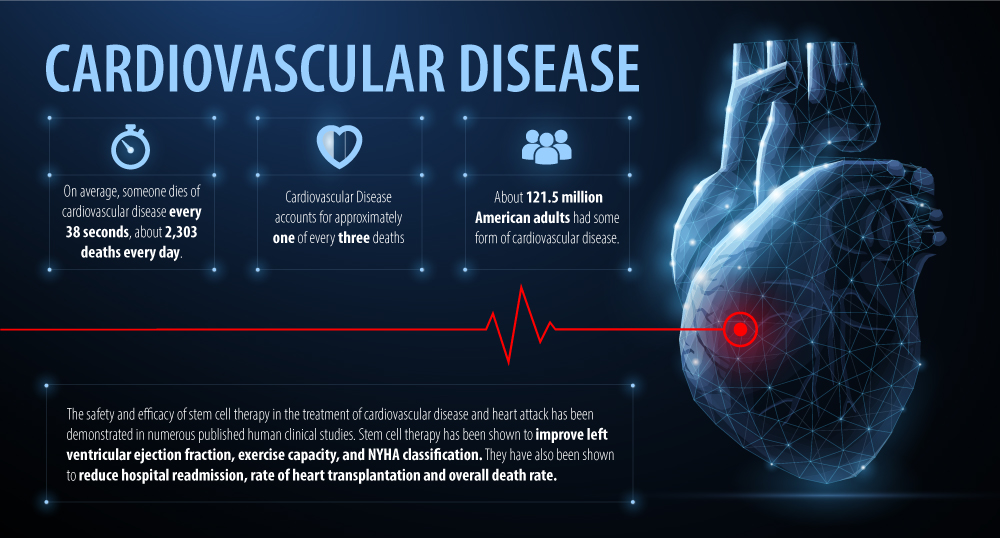
Cardiovascular disease is the leading cause of death worldwide, accounting for more than 17 million deaths per year. Conventional treatments such as surgery and medication have provided some benefit to reduce symptoms, improve clinical indices, slow progression of disease and increase survival. However, despite significant advances in medicine the death toll from cardiovascular disease continues to rise and is expected to grow to more than 23 million by 2030. As such, the search for more effective and safer treatment is on-going among patients, clinicians and researchers.
Stem Cell Therapy and Cardiovascular Disease
Stem cells have been a major area of focus in various cardiovascular conditions including heart failure, cardiomyopathies, heart attack and others due to their powerful properties including anti-inflammatory benefits with the addition of a growing number of human clinical studies showing safety and efficacy.
Stem cells have been shown to have the ability to self-replicate, differentiate into heart muscle cells, prevent fibrosis, reduce inflammation, and induce growth of new blood vessels among other biological effects. These effects have been shown to improve cardiac function and clinical indices, alleviate structural changes in the heart, improve survival and quality of life and reduce occurrence of re-hospitalization.
The vast majority of published clinical studies on stem cell therapy and cardiovascular conditions use stem cells derived from bone marrow tissue. However, due to the invasiveness of the procedure to harvest bone marrow stem cells there is growing interest in other cell types. Umbilical derived stem cells are gaining more attention due to proven efficacy and the ease and accessibility of obtaining such stem cells.
Stem cells can be administered using a variety of methods to treat cardiovascular conditions. The most common methods used in clinical studies include injections into blood vessels of the heart, injections into heart muscles and less commonly intravenous application. However, intravenous delivery of stem cells is gaining more attention due to its ease of application, safety, and efficacy as demonstrated by the RIMECARD trial, a landmark trial of intravenous stem cell therapy and heart failure by Bartolucci et al and the randomized control trial conducted by Butler et al.
Based on early human clinical trials there appears to be a strong argument for the safe and effective use of stem cell therapy in the treatment of cardiovascular disease and heart attack. While we wait for phase II/III trials the current data is encouraging and supports use of stem cell therapy in the clinical setting.
Intravenous Stem Cells and Cardiovascular Disease
| Year | Author | No. of Patients | Cell Type | Delivery | Safety Outcome | Efficacy Outcome |
| 2017 | Bartolucci et al | 30 | UC-MSCs | IV | No acute AEs associated with treatment. No significant differences in AEs between placebo and treatment group. No significant abnormalities were seen in complete blood counts, renal and liver function. | Improvement in LVEF, NYHA and MLHFQ at all follow up points. Improvement in VE/CO2 at 12 months and BNP at 3 and 12 months. |
| 2017 | Bulter et al | 22 | itMSCs | IV | No major differences in death, hospitalization or serious adverse events between groups. There was one treatment related adverse event related to bruising at intravenous infusion site. | LVEDV and LVESV were significantly decreased and the LVEF was improved within the itMSC group when compared to baseline. Statistically significant improvements were observed in health status and functional capacity as measured by changes in KCCQ and in 6MWD at 90 days. |
| 2016 | Fang et al | 3 | UC-MSCs | IV | No complications, AEs or SAEs during and post UC-MSC treatment. No cases of distal coronary artery occlusion, acute cardiac dysfunction, and ventricular arrhythmia occurred. | Increase in LVEF in 2 patients at 3 and 12 months. Significant improvement in 6MWT in two patients. NYHA class improvement was observed in all the patients. |
| 2015 | Chullikana et al | 22 | BM-MSCs | IV | AEs were similar between stem cell and placebo group. No treatment related AEs and no SAEs occurred in patients who received stem cell therapy. | LVEF using echocardiography was improved by almost 5% at 6 months in stem cell group. Perfusion score and size of infarct was not significantly different between the two groups. |
| 20019 | Hare et al | 53 | BM-MSCs | IV | Rates of AEs between treatment and placebo group were similar and no differences in laboratory values for kidney and liver function were observed. | Treatment increased LVEF and reversed remodeling of left ventricle. In stem cell group episodes of ventricular tachycardia was reduced, pulmonary function tests were improved and global symptom scores were significantly increased. |
* UC-MSCs = umbilical cord derived mesenchymal stem cells, IV = intravenous, AEs= adverse events, SAEs = serious adverse events, LVEF = left ventricular ejection fraction, LVESV = left ventricular end systolic volume, LVEDV = left ventricular end-diastolic chamber, 6MWT = 6 minute walk test, NYHA = New York heart association functional classification, MLHFQ = Minnesota living with heart failure questionnaire, BNP = brain natriuretic peptide, itMSC = ischemic tolerant mesenchymal stem cell, BM-MNCs = bone marrow derived mononuclear cells.
Heart Attack and Heart Failure Systematic Reviews
| Year | Author | No of Studies | No. of Patients | Cell Type | Delivery | Follow-up | Safety Outcome | Efficacy Outcome |
| 2019 | Jayaraji et al | 6 RCTs | 526 | Mixed | Mixed | NR | No difference in risk for all-cause mortality between treatment and control groups. | Stem cell therapy statistically significantly improved LVEF by 4.58% and LVESV by -5.18 ml. |
| 2019 | Fan et al | 9 RCTs | 612 | Mixed | Mixed | 6-12 months | Lower incidence of AEs in allogeneic group. | Treatment improved 6MWT by 40.44 m and LVEF by 5.25%. Overall death reduced rate by 36% and hospital readmission by 34%. |
| 2019 | Wang et al | 14 RCTs | 669 | Mixed | Mixed | 2-24 months | No effect on mortality. | Stem cell therapy significantly lowered the NYHA class, LVESV and CCS grade. LVEF was significantly increased (MD = 6.55). LVEDV and mortality did not differ between treatment and control groups. |
| 2018 | Lalu et al | 23 -11 AMI -12 IHF |
1,148 -509 AMI -639 IHF |
Mixed | Mixed | -AMI 6-60 months -IHF 6-36 months |
No association between MSCs and acute adverse events in all studies. No difference in risk of mortality between treatment and control groups. | MSCs increased LVEF compared to controls. Significant improvement in the 6MWT between the MSC group and control for both AMI and IHF. Mixed results of impact on quality of life and NYHA. |
| 2017 | Alp et al | 7 | 345 | UC-MSCs | Mixed | 6-24 months | All studies reported no adverse effect differences between treatment and control groups. | UC-MSC treatments were safe and efficient in restoring cardiac function in a relatively short post-transplantation period. |
| 2016 | Nguyen et al | 29 RCT trials and 7 systematic reviews | 2,817 | Mixed | Mixed | 4-60 months | Arrhythmias reported in 2 studies in heart failure. | Mixed results on impact on LVEF. An overall modest benefit in patients receiving stem cell therapy. |
| 2016 | Fisher et al | 38 RCTs | 1,907 | Mixed | Mixed | 1-120 months | Few SAEs reported during mapping or injection procedure. SAEs early postoperative were rare. AEs associated with bone marrow aspiration were rare. | BM-MSCs reduced mortality and improve LVEF over short‐ and long‐term follow‐up, and may reduce the incidence of non‐fatal MI and improve NYHA in people with chronic IHD and CHF. (Low quality evidence) |
* CTs = randomized controlled trials, NR = not reported, LEVF = left ventricular ejection fraction, LVESV = left ventricular end systolic volume, AEs = adverse events, SAEs = serious adverse events, LVEDV = left ventricular end-diastolic chamber, 6MWT = 6 minute walk test, MD = mean deviation, NYHA = New York heart association functional classification, CCS grade = Canadian cardiovascular society angina grade, HF = heart failure, IHD = ischemic heart disease, CHF = congestive heart failure, AMI = acute myocardial infarction, UC-MSC = umbilical cord derived mesenchymal stem cell, BM-MNCs = bone marrow derived mononuclear cells.
Cardiomyopathy Systematic Reviews
| Year | Author | No of Studies | No. of Patients | Cell Type | Delivery | Follow-up | Safety Outcome | Efficacy Outcome |
| 2019 | Rong et al | 8 RCTs | 531 | Mixed | Mixed | 12-60 months | No significant differences in mortality between treatment and control groups. | Stem cell therapy significantly improved LVEF and significantly reduced LVESV and LVEDV size. Stem cell therapy did not have an effect on mortality and 6MWT. |
| 2018 | Wen et al | 7 RCTs | 463 | BM-MNCs | Mixed | 15-60 months | BM-MNCs had no impact on the risk of all cause death. | BM-MNCs significantly improved LVEF by 3.79%. Effects on LVEF were sustained as demonstrated by a more significant improvement in patients with longer follow up of 15 months to 5 years. |
| 2016 | Lu et al | 7 RCTs | 482 | BM-MNCs | IC and IM | > 12 months | NR | Stem cell therapy had a significant reduction in mortality rates, began to have improvements in LVEF within 6 months and had significantly improved LVEF between 6-12 months. Stem cell therapy also reduced LVESV between 6-12 months. There were no significant changes in 6MWT. |
| 2014 | Jiao et al | 7 RCTs | 599 | Mixed | IC | 3-60 months | NR | Patients who received stem cell therapy had significantly increased LVEF by 3.98%, improved 6MWT, reduced mortality and reduced rate of heart transplantation. |
* RCTs = randomized controlled trial, LVEF = left ventricular ejection fraction, LVESV = left ventricular end systolic volume, LVEDV = left ventricular end-diastolic chamber, 6MWT = 6 minute walk test, BM-MNCs = bone marrow derived mononuclear cells, NR = not reported, IC = intracoronary injection, IM = intramyocardial injection
Early Human Clinical Trials of Stem Cells in Cardiovascular Disease and Heart Attack:
Cardiomyopathy
- Improvement in left ventricular end-systolic volume (LVESV) and left ventricular end-diastolic chamber size (LVEDV) in patients with dilated cardiomyopathy (Rong et al)
- Improvement in left ventricular ejection fraction (LVEF) in patients with dilated cardiomyopathy (Rong et al, Jiao et al)
- Significant improvement in left ventricular ejection fraction (LVEF) in patients with non-ischemic dilated cardiomyopathy (Wen et al, Lu et al)
- Significant reduction in mortality rates in patients with non-ischemic dilated cardiomyopathy (Lu et al)
- Improvement in exercise capacity measured by 6 minute walking test (6MWT) in patients with dilated cardiomyopathy (Jiao et al)
- Reduced rate of heart transplantation in patients with dilated cardiomyopathy (Jiao et al)
Heart Failure
- Improvement in left ventricular ejection fraction (LVEF) in patients with heart failure (Jayaraj et al, Bartolucci et al, Wang et al)
- Reduction in overall death rate and hospital readmission in patients with systolic heart failure (Fan et al)
- Improvement in exercise capacity measured by 6 minute walking test in patients with systolic heart failure (Fan et al)
- Reduction in NYHA classification in patients with ischemic heart failure (Fan et al, Wang et al, Bartolucci et al)
Heart Attack
- Improvement in left ventricular ejection fraction (LVEF) in patients with acute heart attack (Lalu et al, Chullikana et al, Hare et al)
- Significant improvement in exercise capacity measured by 6 minute walking test (6MWT) in patients with acute heart attack (Lalu et al)
- Reversed remodeling of left ventricle in patients with acute heart attack (Hare et al)
- Reduction in episodes of ventricular tachycardia and improved pulmonary function tests in patient with acute heart attack (Hare et al)
Specific Conclusions From Selected Systematic Reviews:
“This meta-analysis suggests that stem cell therapy improves left ventricular ejection fraction and reduces left ventricular end-systolic volume and left ventricular end-diastolic chamber size in patients with dilated cardiomyopathy. However, future well-designed large studies might be necessary to clarify the effect of stem cell therapy in patients with dilated cardiomyopathy.”
- Efficacy and safety of stem cell therapy in patients with dilated cardiomyopathy: a systematic appraisal and meta-analysis (Rong et al)
“Results suggest that stem cell therapy was associated with a moderate improvement in LVEF, and the safety analysis indicates no increased risk of mortality in patients with advanced heart failure.”
- Efficacy and Safety of Stem Cell Therapy in Advanced Heart Failure Patients: A Systematic Review with a Meta-analysis of Recent Trials Between 2017 and 2019 (Jayaraj et al)
“Our results suggested that MSC treatment is an effective therapy for HF by improving the prognosis and exercise capacity.”
- Efficacy of mesenchymal stem cell therapy in systolic heart failure: A systematic review and meta-analysis (Fan et al)
“This meta-analysis suggests that stem cell transplantation is a safe and effective treatment option for patients with IHF since SCT resulted in a reduction in the NYHA class, CCS grade, and LVESV, as well as an increase in LVEF, but did not affect mortality.”
- Effect of stem cell transplantation on patients with ischemic heart failure: A systematic review and meta-analysis of randomized controlled trials (Wang et al)
“There was a significant improvement in overall LVEF in patients who received MSCs” and “Results from our systematic review suggest that MSC therapy for ischemic heart disease appears to be safe.”
- Safety and Efficacy of Adult Stem Cell Therapy for Acute Myocardial Infarction and Ischemic Heart Failure (SafeCell Heart): A Systematic Review and Meta-Analysis (Lalu et al)
“Bone marrow-derived mononuclear cells transplantation is associated with a moderate, but significant, improvement in LVEF in patients with nonischaemic DCM.”
“Safe delivery of cells has been demonstrated in both preclinical and clinical trials” and “Physicians should be aware of the current status of this treatment so that they can better inform their patients who may be in search of alternative therapies.”
- Adult stem cell therapy and heart failure, 2000 to 2016: A systematic review (Nguyen et al)
“This systematic review and meta-analysis found low-quality evidence that treatment with bone marrow-derived stem/progenitor cells reduces mortality and improves left ventricular ejection fraction over short- and long-term follow-up and may reduce the incidence of non-fatal myocardial infarction and improve New York Heart Association (NYHA) Functional Classification in people with chronic ischaemic heart disease and congestive heart failure.”
- Stem cell therapy for chronic ischaemic heart disease and congestive heart failure. (Fischer et al)
“Bone marrow-derived stem cell therapy might have improved prognoses and appeared to provide moderate benefits in cardiac systolic function at mid-term follow-up.”
- A systematic review of randomised controlled trials examining the therapeutic effects of adult bone marrow-derived stem cells for non-ischaemic dilated cardiomyopathy (Lu et al)
“Our study “demonstrated that stem cell therapy improves cardiac function and reduces mortality in dilated cardiomyopathy patients, which suggested that stem cell therapy may represent a new therapy option for dilated cardiomyopathy.”
- Effects of stem cell therapy on dilated cardiomyopathy (Jiao et al)
Specific Conclusions From Selected Studies:
“Intravenous infusion of UC-MSC was safe in this group of patients with stable heart failure and reduced ejection fraction under optimal medical treatment. Improvements in left ventricular function, functional status, and quality of life were observed in patients treated with UC-MSCs.”
- Safety and efficacy of the intravenous infusion of umbilical cord mesenchymal stem cells in patients with heart failure: A phase 1/2 randomized controlled trial (RIMECARD trial [Randomized clinical trial of intravenous infusion umbilical cord mesenchymal (Bartolucci et al)
“This study shows that despite low myocardial engraftment, intravenously administered MSCs improve clinical end points, effects possibly caused, in part, by systemic anti-inflammatory effects”. “Overall, this study found a single dose of intravenous itMSCs to be safe, to be well-tolerated, and to provide clinically relevant signals for efficacy.”
- Intravenous Allogeneic Mesenchymal Stem Cells for Nonischemic Cardiomyopathy: Safety and Efficacy Results of a Phase II-A Randomized Trial (Butler et al)
“[Stem cell] therapy is a reasonable salvage treatment in HF” and due to their small study population “future large scale randomized clinical trials are likely to be designed to elucidate the efficacy.”
- Intravenous Allogeneic Mesenchymal Stem Cells for Nonischemic Cardiomyopathy: Safety and Efficacy Results of a Phase II-A Randomized Trial (Fang et al)
“This study showed that Stempeucel was safe and well tolerated when administered intravenously in AMI patients 2 days after percutaneous coronary intervention.”
- Randomized, double-blind, phase I/II study of intravenous allogeneic mesenchymal stromal cells in acute myocardial infarction. (Chullikana et al)
“Intravenous allogeneic hMSCs are safe in patients after acute MI.”
- A Randomized, Double-Blind, Placebo-Controlled, Dose-Escalation Study of Intravenous Adult Human Mesenchymal Stem Cells (Prochymal) After Acute Myocardial Infarction (Hare et al)
For additional information and details regarding these studies please visit our Research Archives.
Exosomes have potential significant therapeutic effects in regenerative medicine, anti-aging and chronic disease. Click here to learn more about Exosome Therapy.
Brought to you by:
Ahvie Herskowitz, MD, President of ACAM
Director of Anatara Medicine
Clinical Professor of Medicine at UC San Francisco (2014)
(Read Dr. Herskowitz’s Bio Here)
Disclaimer
The contents of Understanding Stem Cells, such as text, graphics, images and other materials are for educational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis or treatment. You are encouraged to confirm any information on this website with other sources and review all information regarding any medical condition or treatment with your physician.
View our Terms and Conditions