Conditions
Orthopedic
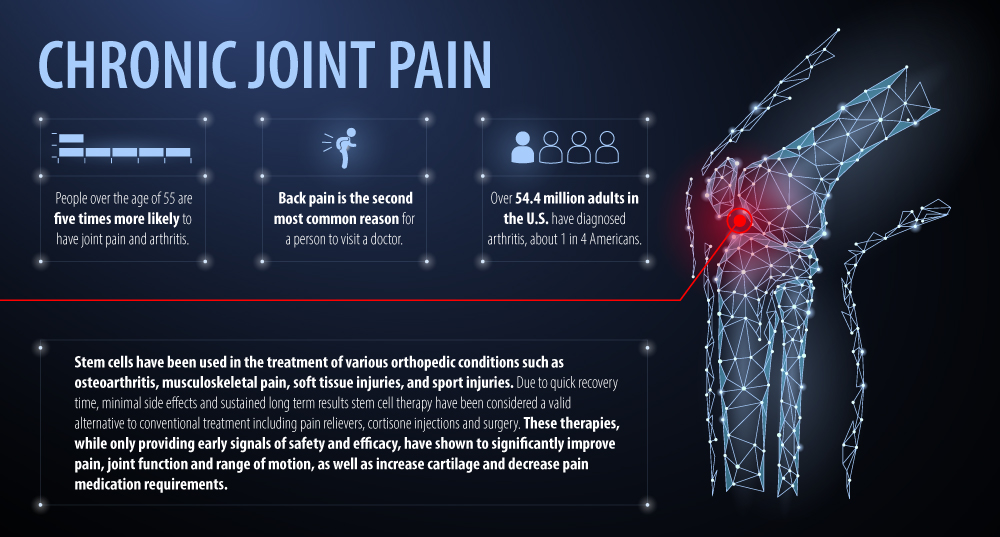
Conventional treatment using over the counter and prescription pain medications are commonly used to reduce symptoms, however have been shown to have significant side effects when used long term. Cortisone injections are also a commonly used conventional treatment to reduce pain and inflammation, but also have significant side effects. Furthermore, cortisone injections do not stimulate the repair of injured tissue. Surgery and/or joint replacement can be beneficial but are associated with potential surgery related complications and often involves a lengthy recovery time of many weeks if not months.
One less conventional option is Platelet Rich Plasma (PRP), which is gaining popularity for the treatment of various orthopedic conditions such as osteoarthritis, musculoskeletal pain, soft tissue injuries, sport injuries, etc.
Unlike medications, cortisone injections, and surgery, nonconventional options like PRP or human cellular tissue products have shown to reduce pain, inflammation and assist with function. In addition, studies show patients often find they are able to reduce their use of over the counter and prescription pain medications.
Based on the early human clinical trials we present there appears to be a strong argument for the safe and effective use of stem cell therapy in the treatment of orthopedic conditions. While we wait for phase II/III trials the current data is encouraging and supports use of stem cell therapy in the clinical setting.
Stem Cells in Knee Conditions
| Year | Author | No. of Patients | Delivery and Cell Type | Follow-up | Safety Outcome | Efficacy Outcome |
| 2019 | Freitag et al | 30 | AD-MSCs | 12 months | No SAE documented during 12 month follow up. Two participants experienced severe AE (pain and swelling) | Statistical and clinically significant change in NPRS, WOMAC and KOOS subscale scores. NPRS improved by a percentage of 69% in both treatment groups. Two injection protocol was observed to achieve a trend of greater disease stabilization. |
| 2019 | Hone et al | 16 | AD-SVF | 12 months | No SAEs observed during 12 months. Six patients reported pain and swelling in bilateral knee joints. | VAS pain, WOMAC pain, WOMAC stiffness and ROM significantly improved. WORMS decreased significantly. Statistically significant articular cartilage repair. |
| 2019 | Lee et al | 24 | AD-MSCs | 6 months | No SAES. Treatment-related AEs were reported in eight patients in the MSC group. | All WOMAC sub-scores significantly decreased. The size of cartilage defect of the medial femoral condyle in serial MRI scans remained stable. |
| 2019 | Matas et al | 29 | UC-MSCs | 12 months | No SAEs, deaths, permanent disability, neoplasia, or septic arthritis cases were registered during the trial. Common AEs related to therapy included acute synovitis, knee effusion and pain. | Total WOMAC and WOMAC pain significantly reduced. VAS significantly reduced. MSC groups experienced significant amelioration of pain and disability at 6 and 12 months No change in WORMS score. |
| 2017 | Bansal et al | 10 | AD AVF+PRP | 24 months | No SAEs reported during the 2 year follow-up. One patient reported pain and swelling at injection and liposuction sites. One developed synovitis. | Significant reduction in total WOMAC and subscales of WOMAC. Cartilage thickness improved by at least 0.2 mm in six patients. 6MWD showed statistically significant improvement. Decreased medication requirement. |
| 2017 | Yokota et al | 13 | AD-SVF | 6 months | No SAEs. Pain and swelling at injection and liposuction sites. | JKOM, WOMAC, and VAS were significantly improved at 6 months. |
| 2016 | Pers et al | 18 | AD-MSCs | 6 months | No AEs or SAEs. Laboratory tests, vital signs, and EEG indicated no local or systemic safety concerns. | Improvement in VAS pain and WOMAC and KOOS function. No correlation between MRI and clinical changes. |
| 2015 | Centeno et al | 2,372 | BMC, BMC with adipose graft, cultured-expanded MSCs | 26 months | 325 AEs reported; majority due to post-procedure pain and progress of disease. 38 AEs due to procedure and 10 due to stem cells. Of 38 SAEs, 13 ‘possibly related’ and 4 ‘definitely related’ to procedure. None ‘likely related’ or ‘definitely related’ to stem cells. | NR |
| 2014 | Jo et al | 18 | AD-MSCs | 6 months | Nine patients reported AEs, none were related to treatment. Most common AE was nasopharyngitis. | Improvement in WOMAC scores for pain, stiffness and function. Increased cartilage volume and regeneration of articular cartilage. |
* AD-MSCs = adipose derived mesenchymal stem cells, UC-MSCs = umbilical cord derived mesenchymal stem cells, PRP = platelet rich plasma, AEs = adverse events, SAEs= serious adverse events, NPRS = numerical pain rating scale, WOMAC = Western Ontario and McMaster universities osteoarthritis index, KOOS = Knee injury and osteoarthritis outcome score, VAS =Visual analog scale, AD-SVF = Adipose derived stromal vascular fraction, WORMS = Whole-Organ Magnetic Resonance Imaging Score, 6MWD = 6 minute walking distance, JKOM = Japanese Knee Osteoarthritis Measure, EEG = electroencephalogram, NR = not reported.
Stem Cells in Shoulder Conditions
| Year | Author | No. of Patients | Delivery and Cell Type | Follow-up | Safety Options | Efficacy Outcome |
| 2018 | Kim et al | 24 | BMAC + PRP | 3 months | No side effects during bone marrow aspiration or injection of BMAC-PRP, and no complications in the follow-up period. | After 3 months pain and functional outcome scores were significantly improved in injection group however there were no changes in tear size between groups. |
| 2018 | Jo et al | 18 | AD-MSCs | 6 months | Intratendinous injection of AD-MSCs was not associated with adverse events. | Stem cells significantly reduced shoulder pain by 71% in high dose group, improved clinical outcome scores and reduced bursal-sided defect up 90% in high dose group. |
| 2017 | Kim et al | 70 | AD-MSCs | 28 months | None reported | Significant improvements in flexion and external rotation were at final follow up. Patients treated with stem cells had a lower rate of failed healing compared to control group at 1 year follow up. |
| 2015 | Centeno et al | 102 | BMAC | 2 years | No significant treatment-related adverse events reported. | Pain and functional outcome scores were significantly improved at 1 month and up to 2 years. These changes were associated with an average subjective improvement of 48.8%. |
* AD-MSCs = adipose derived mesenchymal stem cells, BMAC = bone marrow aspirate concentration, PRP = platelet rich plasma, AEs = adverse events, SAEs= serious adverse events.
Stem Cell Therapy System Review
| Year | Author | No. of Studies | No. of Patients | Delivery and Cell Type | Follow-up | Safety Options | Efficacy Outcome |
| 2019 | Kim et al | 5 | 220 | MSC | NR | NR | VAS score and Lysholm score, but not WOMAC improved. No significant difference in cartilage repair. |
| 2019 | Ha et al | 17 | 356 | Mixed | 12-84 months | NR | Overall improvement in cartilage repair and or status. Improved or significantly better clinical outcomes in 15 studies. |
| 2018 | Jevotovsky et al | 14 | 288 | Mixed | 6-24 months | SAEs in two patients; synovial effusion and unstable angina. | Improvements in VAS and WOMAC scores. Radiological improvements in 3 studies. |
| 2018 | Iijima et al | 35 | 2,385 | Mixed | 3-60 months | NR | Improvements in VAS, self-reported physical function, cartilage volume and quality. |
| 2018 | Park et al | 10 | 225 | ADSCs | 1.5-24 months | NR | Improvements in VAS, WOMAC and structural outcomes on MRI. |
* NR = not reported, WOMAC = Western Ontario and McMaster universities osteoarthritis index, VAS =Visual analog scale, SAEs= serious adverse events, ADSCs = adipose derived stem cells.
EARLY HUMAN TRIALS OF STEM CELLS WITH ORTHOPEDIC CONDITIONS:
- Significant improvement in pain in people with knee osteoarthritis (Freitag et al, Lee et al, Pers et al, Jo et al, Yokota et al, Matas, Iijima et al)
- Significant improvement in joint function in people with knee osteoarthritis (Freitag et al, Lee et al, Pers et al)
- Regeneration of articular cartilage and increased cartilage volume in people with knee osteoarthritis (Jo et al)
- Significant cartilage repair and improved cartilage thickness in patients with knee osteoarthritis (Hong et al, Bansal et al)
- Decreased pain medication requirement in patients with knee osteoarthritis (Bansal et al)
- Improved cartilage defects and range of motion in patients with hip osteoarthritis (Mardones et al)
- Effective in managing local and radiating low back pain originating from intervertebral discs, facet joints and sacroiliac joints (Sanapati et al)
- Significant improvement in pain, function and overall subjective improvement in patients with lower back pain and disc degeneration (Centeno et al)
- Significant improvement in pain, range of motion and strength in people with thumb osteoarthritis (Murphy et al)
- Superior tendon healing and quality of repaired tendon in people receiving stem cell therapy with rotator cuff surgery (Hernigou et al)
- Significant improvement in pain and function in patients with rotator cuff injury (Kim et al, Centeno et al, Jo et al)
For additional information and more details regarding research and studies please visit see our RESEARCH ARCHIVE.
Exosomes have potential significant therapeutic effects in regenerative medicine, anti-aging and chronic disease. Click here to learn more about Exosome Therapy.
Brought to you by:
Ahvie Herskowitz, MD, President of ACAM
Director of Anatara Medicine
Clinical Professor of Medicine at UC San Francisco (2014)
(Read Dr. Herskowitz’s Bio Here)
Disclaimer
The contents of Understanding Stem Cells, such as text, graphics, images and other materials are for educational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis or treatment. You are encouraged to confirm any information on this website with other sources and review all information regarding any medical condition or treatment with your physician.
View our Terms and Conditions